Veracity InSight – Payer Reporting, Appeal Statuses and Denial/Audit Data Visualization at Your Fingertips
Veracity’s intuitive payer denial/audit/appeal visualizations feed you and your team actionable steps to improve workflow performance and identify payer or internal behaviors leading to increasing denials and audits. Keep on top of Work Productivity, Payer Audit Results, Coding Reviews, Denied Dollars by Payer, Physician and Department, Payer Denial Trending, and much more.
- Codes Review Reporting
- Trending Reports
- Root Cause Data
- Task Productivity
- Dashboard Data Visualization
- Automatic Report Scheduler
- Data Drill-Down
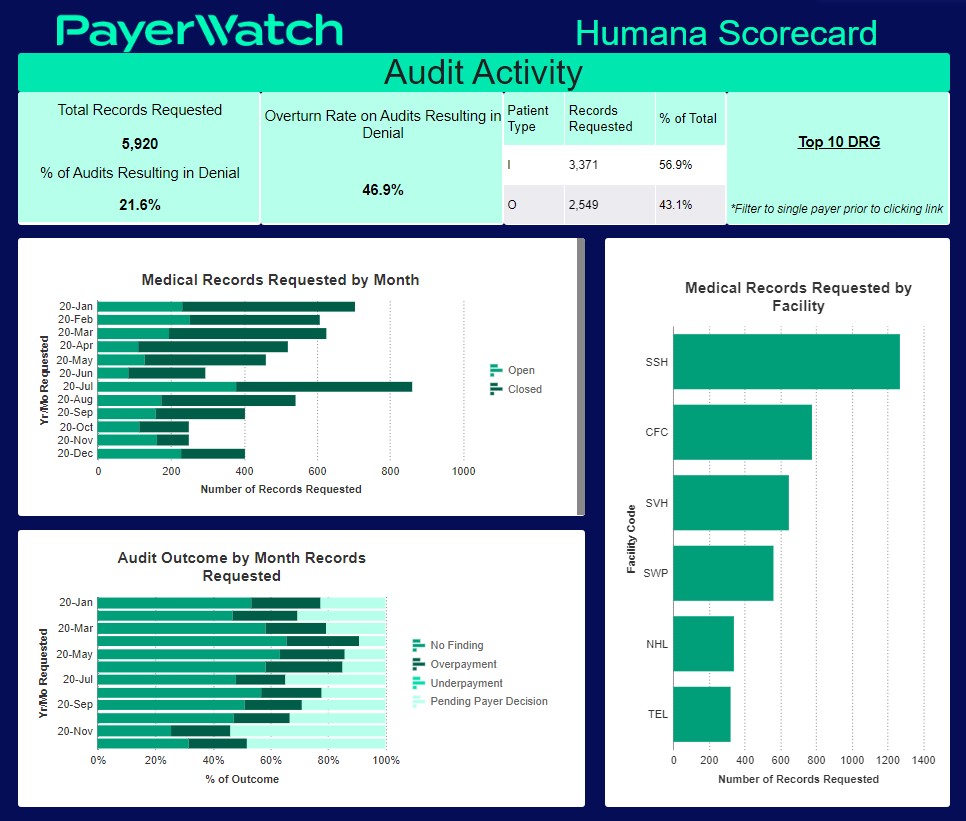
Detailed Analytics
PayerWatch’s Veracity software provides your teams with detailed analytics to manage all aspects of the denial, audit, and appeal process.
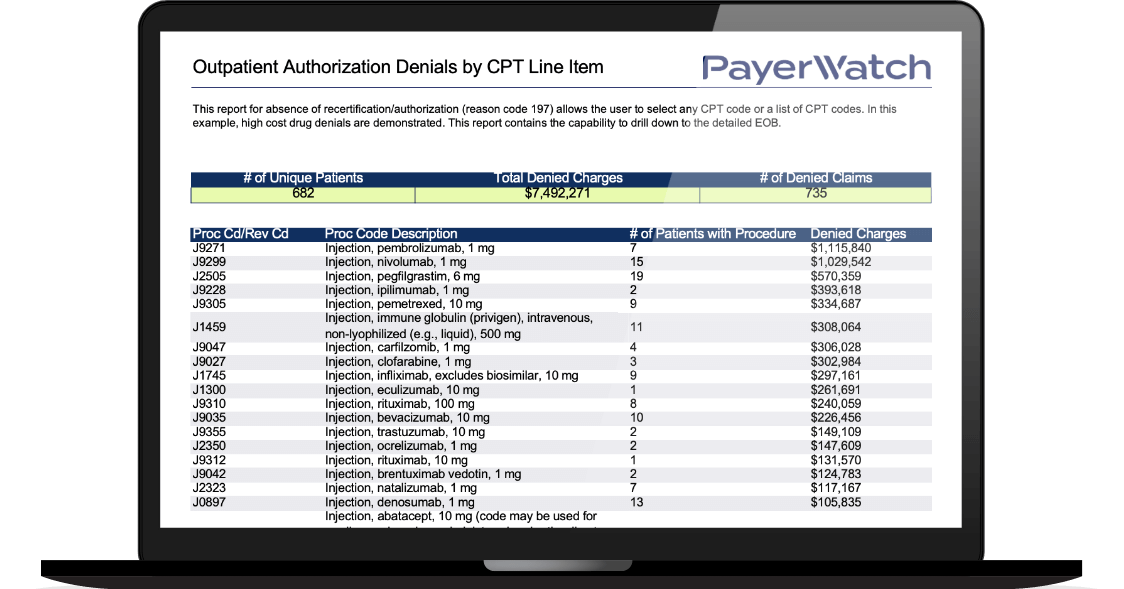
This absence of a recertification/authorization report (reason code 197) allows the user to select any CPT code or a list of CPT codes. In this example, high-cost drug denials are demonstrated. This report contains the capability to drill down to the detailed EOB.
Automated Reports For Analysis
Free up time spent running daily, weekly, monthly or yearly reports by sending them automatically via a secure email.
Drill-down reports identify denial/appeal trends, specific diagnoses/procedures to help reduce claims denials and provide evidence-based reports for appeals.
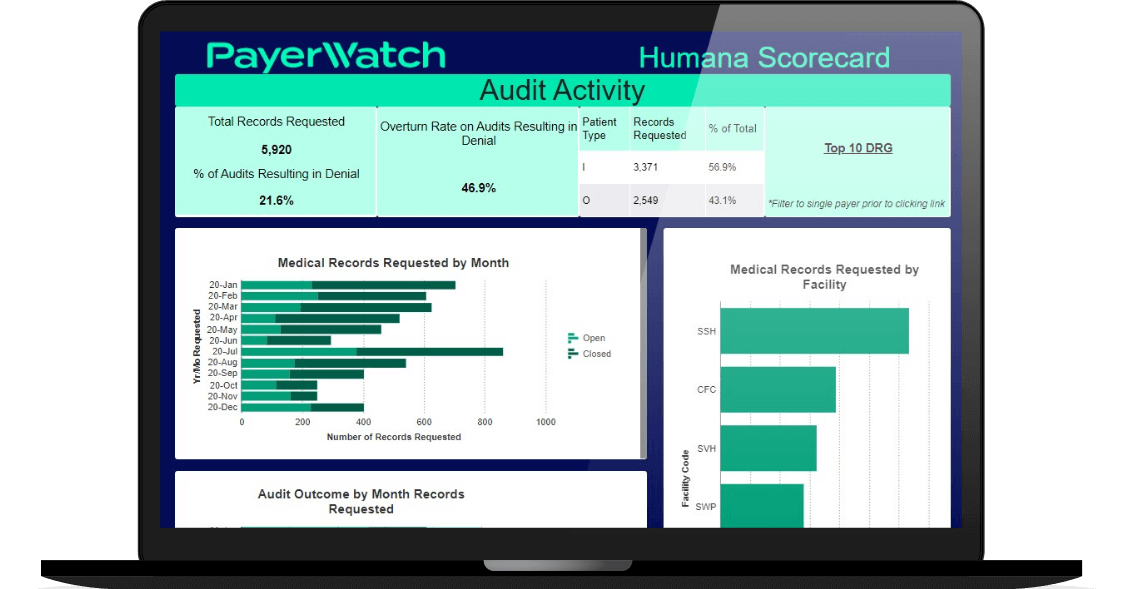
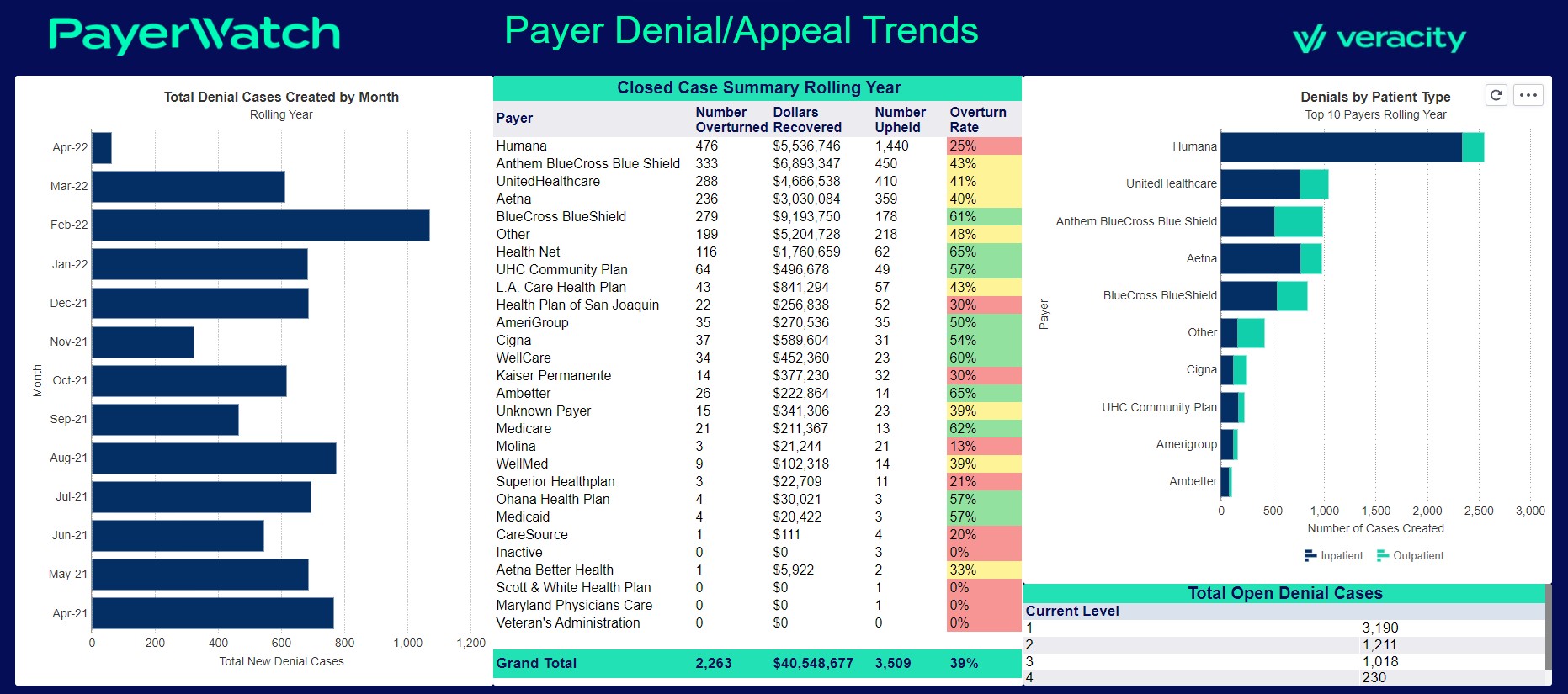
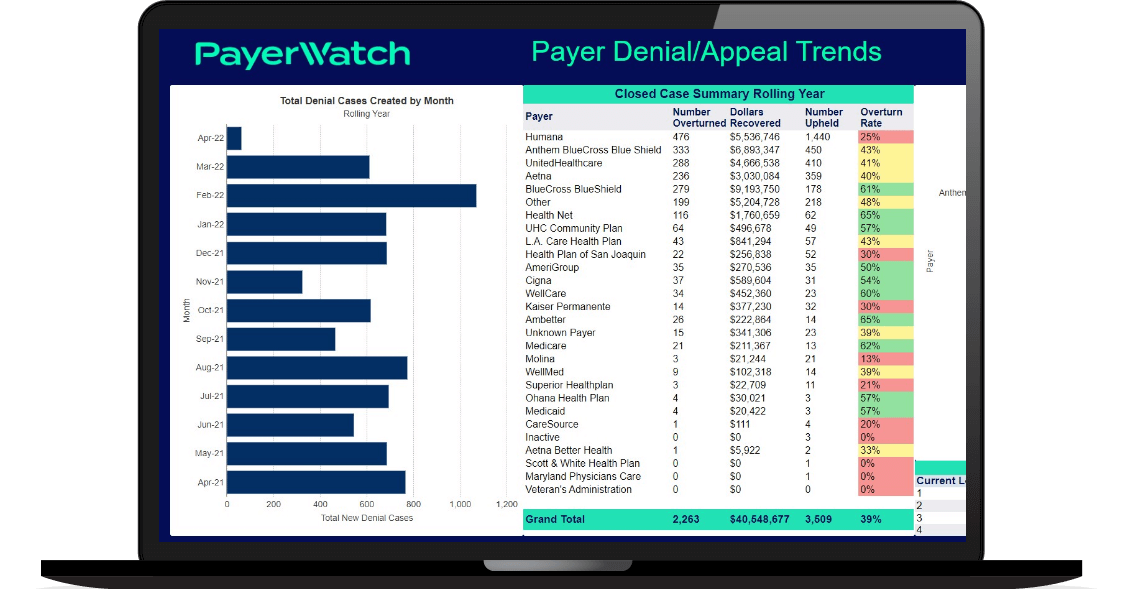
Dashboard Data Visualization
Easily assemble reports into an interactive, customizable Denial | Audit | Appeal dashboard using graphs, charts, text, images, and more.
Your teams will be able to visualize and measure key performance indicators with at-a-glance insights in as much or as little detail as you need.

PayerWatch is a dedicated healthcare provider partner that delivers an enterprise suite of technology, service, and support for denials, audits, and appeals.
Our enterprise Veracity revenue protection engine enables your internal teams with innovative tools at their fingertips. As your revenue protection and defense partner, Veracity comes with ongoing training and customer support, AppealMasters expertise, and education through our Association of Healthcare Denial & Audit Management (AHDAM) community.
We’re Passionate About Helping You Make the Payers Pay
Our high-touch customer service team is always available to help and support everything you need. PayerWatch’s staff are experts in denials, audits, and appeals who deeply understand your challenges and genuinely want to solve your denied claim and audit issues. When you work with us, you get a collaborative partner, not a vendor. Just ask our 500+ hospital clients.

- 30+ years of experience
- Kendall Smith. MD | Chief Medical Advisor
Appeal Support Services
Supplement and aid your internal resources with PayerWatch’s AppealMasters team of denial management and appeal experts.
Training & Support
The Association of Healthcare Denial and Appeal Management (AHDAM) provides professionals with ongoing training and resources led by subject matter experts.
Trusted Partners
PayerWatch has increased revenue for over 500 hospitals.
PayerWatch's industry-leading Veracity software and AppealMasters’ infrastructure is HITRUST CSF Certified.


