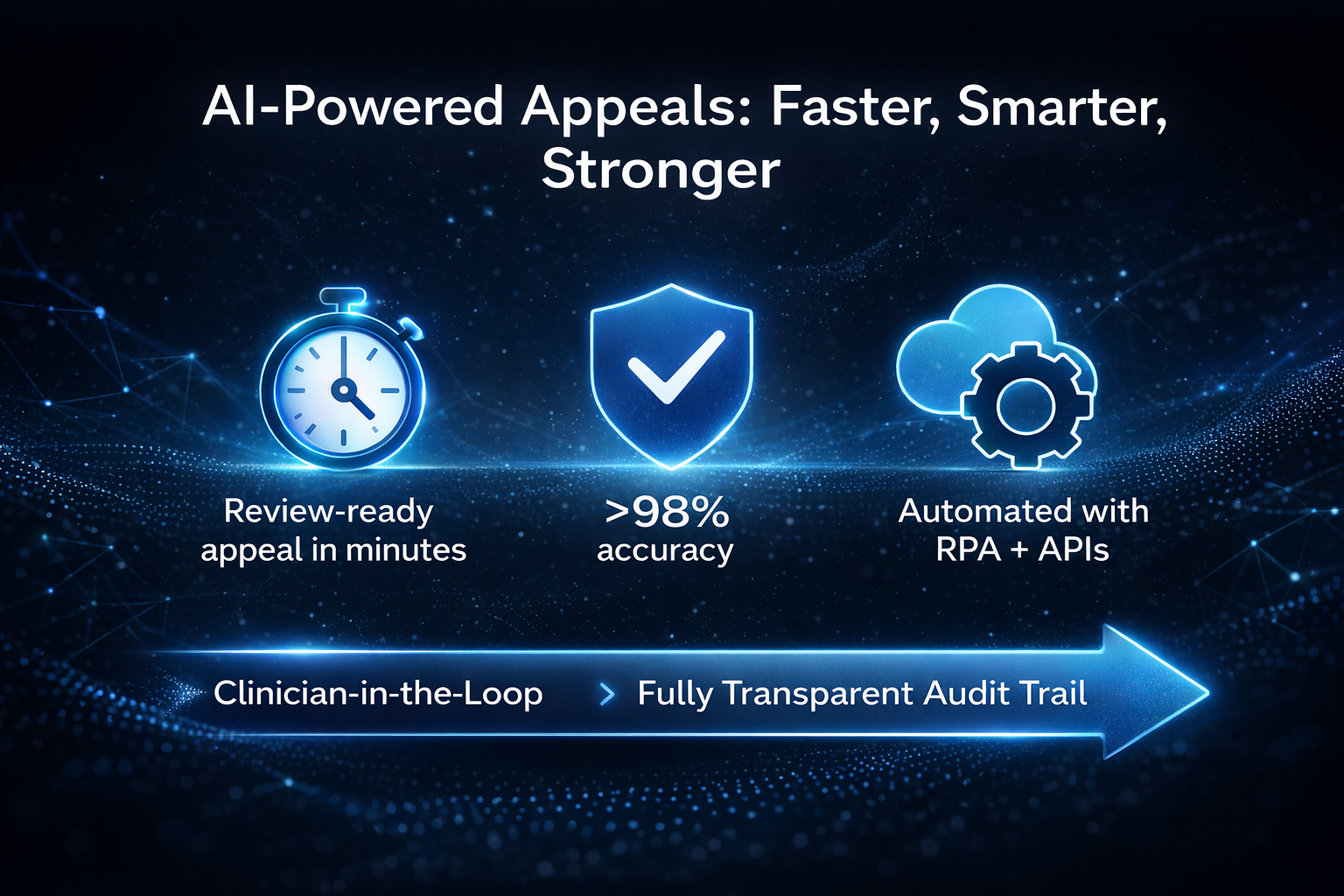
Announcing AI-Assisted Appeals: Veracity delivers first draft appeals in minutes with > 98% accuracy rate on clinical validation, medical necessity, technical, and outpatient denials.
- EMR-agnostic: Works with Epic, Cerner, MEDITECH, and others via current work queues, attachments, secure feeds, and APIs—no re-platforming.
- Human-in-the-loop: Versioned drafts, audit trails, and required clinician verification prior to submission.
- Operationally pragmatic: Automates attachments and submission where technically permitted; supports payer-specific evidence packets.
- Clinically accurate, defensible appeals: No hallucinations; Every fact stated in the letter ties back to specific data in the documentation.
Veracity AI Appeal Engine
Engineered by clinical experts who have spent decades writing appeals, overturning denials, and navigating the complexities payers rely on. It doesn’t just write appeals, it produces defensible, accurate, clinically sound arguments with zero hallucinations.
Enterprise Revenue Risk Management
Veracity provides a unified solution for managing revenue risks across the enterprise—hospitals, clinics, and ancillary services. By centralizing denial and audit responses and tracking, it restores revenue at risk, ensuring a more effective approach to protecting your bottom line.
Flexible workflow engine for quickly fixing broken processes
Identify and fix broken or inefficient revenue cycle processes quickly and effectively across all involved departments. Get it done today, not three months from today.
Preventing Denials to Increase Revenue
Get paid sooner and more often, while drastically reducing the hard and soft costs associated with the administrative burden of audits and denials.
Dedicated appeal experts in your corner
AppealMasters - Our team of specialized clinical-legal appeal experts serve as an extension of your team. As-needed appeal support from initial denial to ALJ hearings and External Review. Training, education, and process improvement recommendations are all included in our appeal support partnership.

PayerWatch is pleased to announce a strategic partnership with Hyve Health, a health data and intelligence platform dedicated to transforming how hospitals track and improve financial and clinical performance.
Through this collaboration, the Vitality Payer Scorecard™—Hyve’s proprietary tool that benchmarks hospital performance across critical revenue cycle and operational metrics—will now be available to clients using PayerWatch’s Veracity™platform.
PayerWatch is the nation’s leading clinical revenue cycle and process improvement solution.
Is your hospital or health system equipped with the strongest tools and denial expert partners to effectively defend yourselves from payer denials and audits? PayerWatch is proven in over 500 hospitals nationwide.

Veracity
Revenue Protection Engine
Denials | Audits | Appeals
Dramatically increase your revenue protection and plug the payer leaks with our Veracity enterprise platform. Guaranteed.
- Denial prevention now
- Rapidly identify and fix broken processes
- Recover more revenue faster with fewer steps
AI That Knows How Appeals Are Won
-
-
Clinically accurate, defensible appeal narratives
-
Built by experts who’ve overturned thousands of denials
-
Structured to meet payer and regulatory standards
-
Tailored by denial type, audit type, and payer logic
-
Fast—without sacrificing accuracy
-

- Clinical Validation Challenges
- Medical Necessity Denials
- Clinical/Legal Unit Approach
- Supporting 500+ Hospitals
PayerWatch Appeal Support Services
Supplement your internal resources with PayerWatch’s AppealMasters team of revenue recovery experts and complex payer appeal services. We’ll continuously train, educate and transfer knowledge as we help you win more appeals faster. Because performance improvement matters.
Advocacy, Training and Support
The Association of Healthcare Denial and Appeal Management (AHDAM) provides ongoing training and resources for all health care providers nationwide. AHDAM offers extensive training and education in denial and appeal management. Led by an expert team of denial and appeal management physicians, nurses, coders and attorneys.
PayerWatch is a fierce advocate for healthcare providers.
We empower you with the most efficient and effective tools to manage abusive payer practices, payer denials, payer audits and a winning appeal process.
Whether you’re leveraging the technological advancements of our Veracity revenue protection engine or supporting your internal teams with our expert AppealMasters support, PayerWatch is your trusted partner for revenue protection and defense. Over 500 hospital clients feel the same.
PayerWatch AppealMasters Experts are Passionate About Making the Payers Pay
Our industry‐leading customer service is available to help and support everything you need to succeed in this incredibly challenging payer-provider environment. The PayerWatch staff are experts in medical necessity, clinical validation/CDI, coding, contracts, and legal protections who deeply understand the issues at hand and can help solve your denial, audit, and payer challenges. You get a serious, educated collaborative, and expert partner. Our Veracity and AppealMasters teams build close working relationships with your staff, who share in the service mission to improve processes and payment outcomes together.
Trusted Partners
PayerWatch has increased revenue for over 600 hospitals.
PayerWatch's industry-leading Veracity software and AppealMasters’ infrastructure is HITRUST CSF Certified.




